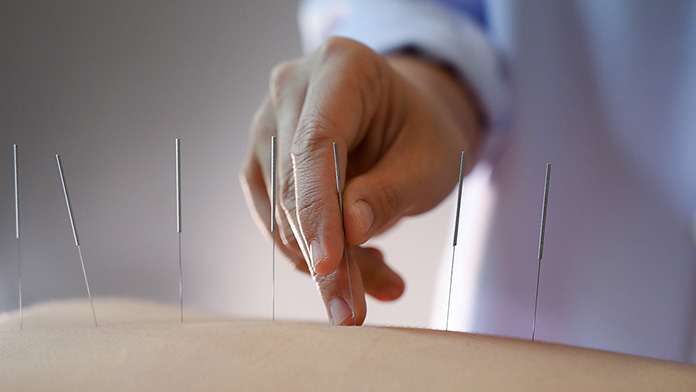
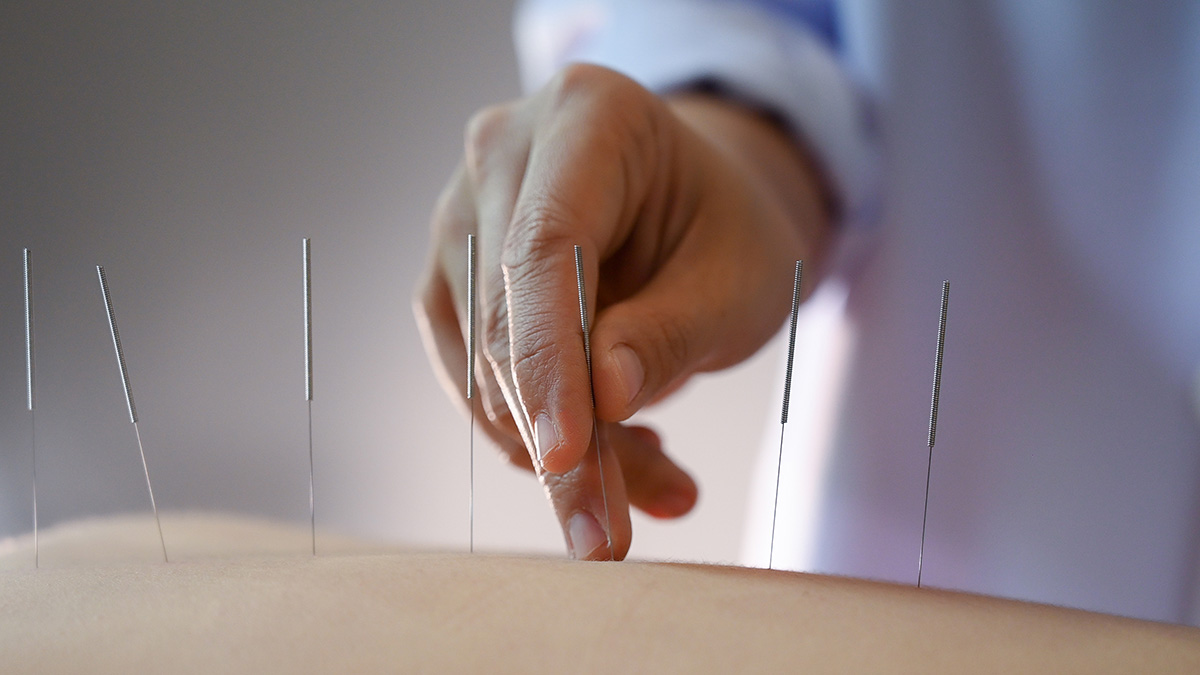
For centuries, Western medicine and traditional healing practices often stood at opposite ends of the health spectrum. Conventional medicine, grounded in scientific methodology, emphasizes pharmaceuticals, surgery, and evidence-based guidelines. Acupuncture, on the other hand, originates from traditional Chinese medicine (TCM) and involves stimulating specific points on the body to restore balance and promote healing. Historically, many physicians viewed acupuncture with skepticism, dismissing it as unscientific or placebo-driven.
Yet over the past few decades, a remarkable shift has occurred. Increasingly, medical doctors are referring patients to licensed acupuncturists. This trend is not an abandonment of science but rather a reflection of a growing body of research, patient demand, and the recognition that healthcare works best when it is holistic. In this article, we will explore in depth the reasons why medical doctors choose to refer their patients to acupuncturists, examining the clinical, psychological, and systemic factors driving this integrative approach.
1. Evidence-Based Support for Acupuncture
Clinical Research and Trials
One of the most compelling reasons physicians now embrace acupuncture is the accumulation of rigorous clinical studies supporting its efficacy. Large-scale meta-analyses and randomized controlled trials have demonstrated that acupuncture is effective for conditions such as chronic pain, tension headaches, migraines, osteoarthritis, and postoperative nausea.
For example:
- A landmark 2012 meta-analysis published in the Archives of Internal Medicine reviewed nearly 18,000 patients and concluded that acupuncture provided significant pain relief beyond placebo.
- The World Health Organization (WHO) and the National Institutes of Health (NIH) have recognized acupuncture as a legitimate therapeutic option for multiple conditions.
This evidence provides doctors with confidence that they are not merely indulging a complementary practice but recommending a scientifically validated treatment.
Neurological Mechanisms
Modern neuroimaging and biochemical studies show that acupuncture stimulates the release of endorphins, serotonin, and dopamine, modulates inflammatory responses, and influences brain regions associated with pain perception. These physiological mechanisms help bridge the gap between Eastern tradition and Western science, making it easier for doctors to justify referrals.
2. Addressing Chronic Pain and the Opioid Crisis
The Burden of Chronic Pain
Chronic pain affects millions of patients worldwide, often leading to disability, reduced quality of life, and increased healthcare costs. Traditional medical approaches—long-term use of painkillers, invasive procedures, or surgery—are not always effective and often come with significant side effects.

The Opioid Epidemic
With the opioid crisis escalating in recent decades, physicians are under pressure to find alternatives that manage pain without addictive risks. Acupuncture has emerged as a viable non-pharmacological solution. Studies have shown it can reduce reliance on opioids, decrease withdrawal symptoms, and improve pain outcomes.
Doctors may refer patients to acupuncturists as part of a broader pain management strategy, aligning with guidelines from organizations such as the American College of Physicians, which recommend non-drug therapies as first-line treatments for chronic low back pain.
3. Holistic Patient Care
Treating the Whole Person
Conventional medicine often excels at diagnosing and treating specific diseases but can fall short in addressing the holistic needs of patients—emotional, psychological, and social. Acupuncture, grounded in TCM philosophy, considers the interconnectedness of body, mind, and spirit. Doctors who refer patients to acupuncturists acknowledge the value of this whole-person approach.
Enhancing Patient Well-Being
Patients frequently report not only symptom relief but also improvements in sleep, mood, digestion, and overall vitality after acupuncture treatments. This aligns with physicians’ broader goal of improving patients’ quality of life, not just managing disease.
4. Patient Demand and Satisfaction
Responding to Patient Interest
In an era of shared decision-making, physicians must consider patient preferences. Many patients seek acupuncture independently or inquire about it after hearing positive testimonials. Rather than dismissing these requests, doctors increasingly choose to refer to licensed practitioners, ensuring patients receive safe, regulated, and effective treatment.
Boosting Trust and Satisfaction
By validating patients’ interest in acupuncture, doctors foster stronger therapeutic alliances. This improves patient satisfaction, compliance, and trust in the healthcare system as a whole. Patients feel heard, respected, and empowered when their doctors support integrative options.
5. Complementing Conventional Treatments
Reducing Side Effects
Acupuncture can help manage the side effects of standard medical interventions. For example:
- Cancer patients undergoing chemotherapy often experience nausea, fatigue, and neuropathy. Studies show acupuncture can alleviate these symptoms, improving tolerance to treatment.
- Post-surgical patients may benefit from acupuncture to reduce pain and accelerate recovery without excessive reliance on opioids.
Enhancing Outcomes
Doctors may refer patients to acupuncturists not as a replacement but as a complement to medical care. Integrative treatment plans often result in better outcomes than either approach alone. For instance, combining physical therapy with acupuncture can accelerate rehabilitation after musculoskeletal injuries.
6. Mental Health and Stress Reduction

Rising Mental Health Needs
Mental health challenges—such as anxiety, depression, and stress-related disorders—are increasingly prevalent. While psychotherapy and medication remain standard treatments, many patients either cannot tolerate medications or prefer non-drug options.
Acupuncture’s Role
Acupuncture has been shown to modulate the autonomic nervous system, reduce cortisol levels, and promote relaxation. Doctors may refer patients seeking stress relief, improved sleep, or adjunctive support for anxiety and depression. The calming effects of acupuncture often complement psychiatric care, offering patients a sense of balance and resilience.
7. Preventive and Lifestyle Medicine
Shifting Toward Prevention
Healthcare is gradually moving from a disease-treatment model to a prevention-oriented paradigm. Acupuncture, with its focus on balance and energy flow, is well-suited to preventive medicine. Regular sessions may help maintain health, boost immunity, and reduce the likelihood of future illness.
Lifestyle Integration
Doctors who advocate for exercise, nutrition, and mindfulness practices often see acupuncture as another valuable tool for preventive health. Referrals in this context support patients in adopting healthier lifestyles and proactively managing stress.
8. Cost-Effectiveness and Healthcare Economics
Lowering Costs
Chronic conditions such as back pain, migraines, and arthritis place enormous burdens on healthcare systems. Surgery, imaging, and long-term medications are costly. Acupuncture, though not inexpensive, often reduces the need for expensive interventions, making it cost-effective in the long run.
Insurance Coverage
As more insurance plans cover acupuncture, referrals become easier for doctors to justify. Patients are more likely to pursue acupuncture if it is financially accessible, further incentivizing physicians to recommend it.
9. Professional Collaboration and Interdisciplinary Care
Integrative Clinics
Many hospitals and medical centers now host integrative medicine departments where acupuncturists work alongside physicians, physical therapists, and dietitians. This collaboration fosters mutual respect and streamlined patient care.
Cross-Referrals
Doctors recognize that acupuncturists bring unique expertise to the healthcare team. Just as they might refer to a cardiologist or physical therapist, they increasingly see acupuncturists as specialists in their own domain. This model reduces fragmentation and improves continuity of care.
10. Cultural Competence and Diversity in Care
Respecting Cultural Practices
In multicultural societies, many patients already use traditional medicine systems, including acupuncture. By acknowledging and integrating these practices, doctors demonstrate cultural competence and inclusivity, which is critical in building trust with diverse patient populations.

Bridging Worlds
Doctors who refer to acupuncturists help bridge Western and Eastern medical paradigms, showing openness to multiple healing traditions. This fosters a more pluralistic healthcare environment where patients’ cultural values are respected.
11. Safety Profile of Acupuncture
Low Risk of Adverse Effects
When performed by licensed practitioners, acupuncture is remarkably safe, with minimal side effects compared to pharmaceuticals or invasive procedures. Common adverse events are usually limited to mild bruising or soreness at needle sites.
Safer Option for Vulnerable Populations
Doctors may refer pregnant women, elderly patients, or those with multiple drug sensitivities to acupuncturists because acupuncture offers a low-risk alternative or adjunct to medication-heavy approaches.
12. Expanding the Definition of Healing
Beyond Symptom Management
While Western medicine often focuses on symptom suppression, acupuncture emphasizes restoring balance and harmony. Doctors who refer to acupuncturists recognize that healing is not merely the absence of disease but the presence of vitality, resilience, and well-being.
Empowering Patients
Acupuncture sessions often create space for patients to reflect, rest, and reconnect with themselves—experiences not always prioritized in conventional medical appointments. This can be profoundly therapeutic and empowering.
Conclusion
The growing trend of medical doctors referring patients to acupuncturists reflects a broader transformation in healthcare. It is driven by a convergence of scientific validation, patient demand, the opioid crisis, and the recognition that holistic, integrative approaches often yield the best outcomes. Acupuncture is no longer seen as an alternative but as a complementary practice that enriches conventional medicine.
By embracing acupuncture as part of an integrative model, doctors are not abandoning science but expanding the definition of evidence-based care. They are acknowledging that healing is complex, multifaceted, and deeply personal. Referrals to acupuncturists embody a future where healthcare is not divided into “Western” and “Eastern” camps but unified by the shared goal of helping patients live healthier, fuller lives

Lee Schwalb is a licensed acupuncturist in New York City with over 20 years of clinical experience, treating a broad range of health issues, from idiopathic pain and acute injuries to stress, anxiety and many other conditions.