
Dry needling is a therapeutic technique used by physical therapists, chiropractors, and other healthcare providers to treat musculoskeletal pain and dysfunction. It involves the insertion of thin, solid needles into myofascial trigger points—tight bands of muscle that can refer pain to other areas of the body. While it is often compared to acupuncture, dry needling is rooted in Western medicine and focuses primarily on the treatment of muscle pain and trigger points. Below is an extensive exploration of how dry needling helps alleviate pain.
1. Understanding Dry Needling
a. Definition
Dry needling targets myofascial trigger points, which are hyperirritable spots in skeletal muscle associated with palpable nodules in taut bands of muscle fibers. These trigger points can cause local and referred pain, leading to a variety of musculoskeletal issues. The technique involves inserting a needle into the skin and muscle without injecting any substance, hence the term “dry.”
b. Historical Context
Dry needling has its origins in the work of Dr. Janet Travell, a physician who extensively studied myofascial pain and trigger points. Her research in the mid-20th century laid the groundwork for the development of this technique. Over the years, dry needling has gained popularity due to its effectiveness in pain management and muscle rehabilitation.
2. Mechanisms of Action
Dry needling is thought to help alleviate pain through several physiological mechanisms. Understanding these mechanisms can provide insight into how this technique works.
a. Trigger Point Deactivation
When a needle is inserted into a trigger point, it can cause a local twitch response, which is an involuntary muscle contraction. This twitch response is believed to help deactivate the trigger point, reducing muscle tension and pain. The mechanical stimulation of the needle may also disrupt the tight bands of muscle fibers, promoting relaxation and improved blood flow.
b. Increased Blood Flow
The insertion of needles into the muscle can enhance local blood circulation. Improved blood flow brings oxygen and nutrients to the tissue while aiding in the removal of metabolic waste products. This can help reduce inflammation and promote healing in the affected muscles.
c. Pain Gate Theory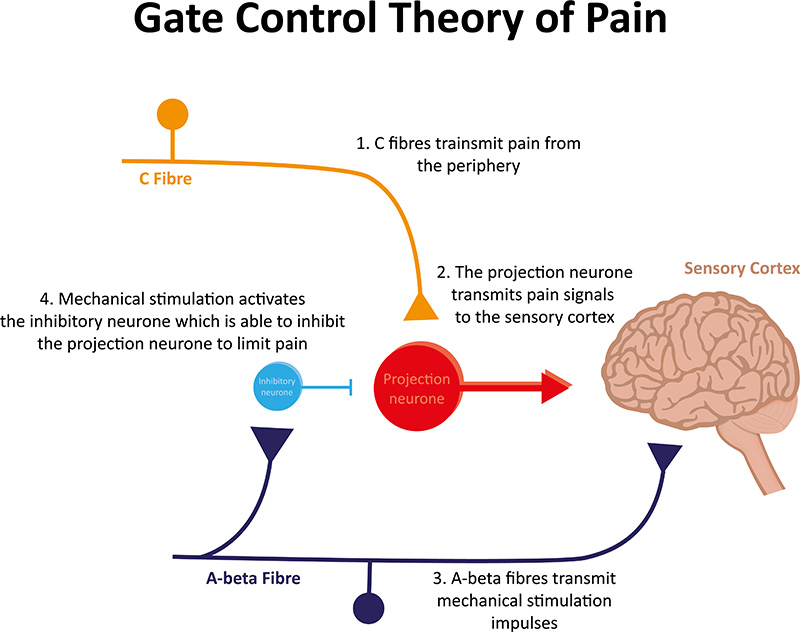
According to the pain gate control theory, the stimulation of sensory fibers by dry needling may help close the “gate” to pain signals being transmitted to the brain. By activating larger sensory fibers, the brain can prioritize these non-painful signals over the pain signals, leading to a reduction in perceived pain.
d. Endorphin Release
Dry needling may stimulate the release of endorphins, the body’s natural painkillers. Endorphins can bind to opioid receptors in the brain, reducing the perception of pain and promoting a sense of well-being.
e. Neuromuscular Re-education
Dry needling can also facilitate neuromuscular re-education. By addressing dysfunctional muscle patterns and trigger points, it can help restore normal muscle function and improve overall movement patterns.
3. Conditions Treated with Dry Needling
Dry needling can be effective for a variety of conditions, particularly those related to musculoskeletal pain. Some common conditions treated include:
a. Myofascial Pain Syndrome
Myofascial pain syndrome is characterized by the presence of trigger points and can lead to chronic pain in specific muscle groups. Dry needling can directly target these trigger points, providing pain relief and improving muscle function.
b. Tension Headaches
Tension headaches can often be linked to tightness in the neck and shoulder muscles. Dry needling can help release tension in these areas, potentially reducing the frequency and intensity of headaches.
c. Chronic Low Back Pain
Low back pain is a common complaint that can be exacerbated by muscle tightness and trigger points. Dry needling can target the muscles in the lower back, providing relief and improving mobility.
d. Sports Injuries
Athletes often develop trigger points due to repetitive movements and muscle strain. Dry needling can help address these trigger points, facilitating faster recovery and improved performance.
e. Neck and Shoulder Pain
Conditions such as cervical radiculopathy and shoulder impingement can benefit from dry needling. By targeting the muscles surrounding these areas, practitioners can alleviate pain and improve range of motion.
4. The Dry Needling Procedure
The dry needling procedure typically involves several steps:
a. Assessment
Before treatment, a thorough assessment is conducted to identify the source of pain and determine the appropriate trigger points to target. The practitioner may ask about the patient’s medical history, perform a physical examination, and assess movement patterns.
b. Needle Insertion
Once the trigger points are identified, the practitioner will insert a thin, sterile needle into the skin and muscle. The depth of insertion may vary depending on the location of the trigger point and the muscle involved. Patients may experience a slight prick or twitch sensation, which is generally well-tolerated.
c. Treatment Duration
Needles are usually left in place for a short duration, typically ranging from a 25-35 minutes. During this time, the practitioner may assess the response of the muscle and make adjustments as needed.
d. Post-Treatment Care
After the session, patients may be advised on post-treatment care, which may include stretching, rest, and hydration. It is common to experience mild soreness in the treated area, similar to post-exercise soreness.
5. Research and Evidence
Numerous studies have explored the effectiveness of dry needling for pain management. Here are some key findings:
– A systematic review published in the *Journal of Orthopaedic & Sports Physical Therapy* found that dry needling was effective in reducing pain and improving function in patients with chronic myofascial pain.
– Another study in the *Archives of Physical Medicine and Rehabilitation* indicated that dry needling significantly reduced pain intensity and improved range of motion in patients with myofascial trigger points.
– Research published in *Pain Medicine* demonstrated that dry needling could provide significant pain relief and functional improvement in patients with chronic low back pain.
6. Safety and Considerations
Dry needling is generally considered safe when performed by trained professionals. However, there are some considerations to keep in mind:
a. Potential Side Effects
Common side effects may include soreness, bruising, or minor bleeding at the insertion site. These effects are usually temporary and resolve on their own.
b. Contraindications
Certain conditions may contraindicate dry needling, including:
– Pregnancy
– Bleeding disorders
– Skin infections
– Recent surgery in the treatment area
It is crucial for practitioners to conduct a thorough assessment to identify any contraindications before proceeding with treatment.
7. Conclusion
 Dry needling has emerged as a valuable technique for managing pain and dysfunction related to musculoskeletal conditions. By targeting myofascial trigger points, it can help deactivate painful muscle knots, improve blood flow, and promote healing. The combination of physiological mechanisms involved in dry needling contributes to its effectiveness in pain relief.
Dry needling has emerged as a valuable technique for managing pain and dysfunction related to musculoskeletal conditions. By targeting myofascial trigger points, it can help deactivate painful muscle knots, improve blood flow, and promote healing. The combination of physiological mechanisms involved in dry needling contributes to its effectiveness in pain relief.
As research continues to support the benefits of this technique, more individuals are discovering the potential of dry needling as part of their pain management and rehabilitation strategies. When combined with other therapeutic modalities, such as physical therapy and exercise, dry needling can play a significant role in helping individuals achieve lasting relief from pain and improved quality of life.
Lee Schwalb is a licensed acupuncturist with over twenty years of clinical experience. He specializes in trigger point/dry needling therapy for musculoskeletal pain disorders.

Lee Schwalb is a licensed acupuncturist in New York City with over 20 years of clinical experience, treating a broad range of health issues, from idiopathic pain and acute injuries to stress, anxiety and many other conditions.

